Welcome Package

Welcome Package
About Our Midwives
Midwives are fully funded by the Ministry of Health and offer free and complete care for you and your newborn. You do not need to see a family doctor or an obstetrician in addition to your midwives. Your midwife will offer all standard prenatal ultrasounds and blood work and is able to prescribe common medications required in pregnancy & postpartum. At The Midwives’ Clinic (TMC), you will have a midwife available to you by pager 24/7 to assist with any urgent concerns. If complications arise, your midwife will initiate the appropriate consultations with a specialist such as an obstetrician, a pediatrician and/or lactation consultant.
Prenatal Care
Prenatal visits include: blood pressure checks, routine tests and assessments of baby’s growth, position and heart rate. Information regarding community programs, resources and referrals are also made available.
Labour & Birth
One midwife is present throughout active labour to assess progress, monitor you and your baby and provide ongoing emotional and physical support. A second midwife will arrive towards the end of your labour to be present for the birth of your baby.
Postpartum
After the birth, both midwives will stay with you for 2-4 hours. They will monitor you and baby, assist with breastfeeding and conduct a complete newborn physical exam. Your midwives will provide home visits in the first week postpartum and appointments in the clinic until your baby is 6 weeks old. Postpartum visits include: initial tests for baby, baby weight checks, postpartum recovery assessments, breastfeeding support and referrals as needed.
Midwifery in Ontario - Governing Bodies
College of Midwives of Ontario
Visit Site or 416-327-0874
The CMO protects the public by regulating the profession of midwifery in accordance with the RHPA and by setting the minimum standard of professional behaviour and clinical practice expected of Midwives in Ontario.
Association of Ontario Midwives
Visit Site or 416-425-9974
The AOM provides services for midwives in Ontario.
Getting to Know your Care Team
YOUR MIDWIVES
For prenatal care, you will have appointments with each of your 2-4 midwives.
Whichever midwife from your team is on call when you go into labour will be the primary midwife at the birth.
YOUR CARE COORDINATOR
Your Care Coordinator is one of your midwives. If you page your midwife with an urgent concern, please ask for your assigned care coordinator. They will make sure one of your midwives responds to you.
THE SECOND MIDWIFE AT YOUR BIRTH
Our goal is that one of the midwives on your team will be with you throughout your active labour and birth. When you are close to delivering, your midwife will call a second midwife who you may or may not have met. The second midwife will assist the primary midwife during the birth. Once the baby is born, the second midwife is there to help care for the baby while the primary midwife continues to look after you.
YOUR THIRD MIDWIFE
A third midwife may be assigned to your team to help cover during busy or off- call times. Sometimes, through unavoidable circumstances such as two births happening at the same time, both of your midwives may be unavailable. Your care coordinator will suggest when these visits should be scheduled.
YOUR STUDENT MIDWIFE
We are a teaching practice that regularly has students from the university based Midwifery Education Program as well as students who have already qualified to practice in other countries but need Ontario experience. Most midwifery clients say that they really benefit from student involvement in their care. Students are always under midwife supervision and participate in clinic appointments, home visits and births. Please talk to your midwives if you have questions or concerns about having a student involved in your care.
About Our Clinic
- You will see a midwife for prenatal visits every 4-6 weeks until 28 weeks, every 2 weeks until 36 weeks and once a week until your baby is born. Due to our on-call schedule, each midwife works only 1-2 clinic days per week. We appreciate client flexibility with regards to appointment scheduling.
- Clinic appointments are typically 30 minutes in length, allowing time for clinical assessments, answering questions and providing information.
- After you give birth, your midwife will provide a home visit within the first 24-28 hours and every few days for the first week. Your midwife will be on-call during this time; therefore some visits may be rescheduled.
- You and your baby will then be seen approximately every 2 weeks at our clinic until 6 weeks postpartum.
- Family members and support people are always welcome!
COMMUNICATING LAB RESULTS
- At TMC, no news is good news!
- All labs are reviewed by a midwife each day to detect any abnormal results.
- In the event of an abnormal lab result or ultrasound, one of your midwives will contact you as soon as possible.
- If you have questions regarding results, please leave a message for your midwife at 416-424-1976.
AT EVERY PRENATAL APPOINTMENT
- Please check in at the front desk and use the washroom at this time if needed.
- Check your weight on the scale in the washroom if you are comfortable doing so. Then let your midwife know the value during your appointment.
CONSULTATIONS & TRANSFERS OF CARE
- If something comes up in pregnancy, labour, birth or postpartum that is outside the midwifery scope of practice, your midwife will recommend a consultation or a transfer of care to the appropriate provider (often an obstetrician).
- The purpose of a consultation is to receive recommendations for your care such as additional testing/monitoring. Most often, you will remain in midwifery care and your midwife will carry out the recommendations.
- Though rare, some clients may require a higher level of care outside the midwifery scope. In the event your care is transferred to a physician, your midwife will offer supportive care including labour support. If the care is transferred back to the midwives in the postpartum period, they will resume normal postpartum care.
- Please see http://www.cmo.on.ca/wp-content/uploads/2015/11/Standard- Consultation-and-Transfer-of-Care-Nov.-2015.pdf for Indications for Discussions, Consultations and Transfers of Care.
Privacy Statement
This includes:
You will be asked to sign a consent form that gives your consent for our collection, use, and disclosure of your personal information for purposes related to your care.
You have the right to see your records. You may also obtain copies of your records – please ask one of your midwives.
Please speak to your midwife if you have any concerns about the accuracy of your records.
If you would like to discuss our privacy policy in more detail or have specific questions or complaints about how your information is handled, please speak to your midwife.
For additional information, you may obtain a copy of our Privacy Policy from our staff.
The Midwives’ Clinic of East York – Don Mills
3-1 Leaside Park Drive Toronto ON M4H 1R1
[www.themidwivesclinic.ca
Paging Service
❖ Excessive vaginal bleeding
❖ Water breaks and umbilical cord is in the vagina or hanging from the vagina.
PAGE IMMEDIATELY
❖ Vaginal bleeding
❖ Severe headache, blurred vision, nausea, vomiting
❖ Severe abdominal pain
❖ Waters break
❖ Decreased or lack of fetal movement
❖ Fever greater than 38.0C/100 degrees Fahrenheit
❖ Regular contractions before 37 weeks of pregnancy
CONTACT OFFICE [416-424-1976]
MONDAY-FRIDAY 9AM-5PM
❖ For discomforts of pregnancy, i.e. backache, rash, indigestion, swelling in feet
❖ To discuss lab results
❖ Urinary tract infection symptoms, pain or burning with urination
Note: Messages will be picked up Monday to Friday 9am-5pm
Please only use pager for immediate concerns or emergencies
PAGER: 416-467-6616 ex: TEAM COLOUR
- If you do not hear back from a midwife within 15 minutes, page again.
- If you still don’t hear back – try another team colour extension
- If you still do not hear back it may be that the paging system is not working. In that case, call the clinic office at 416-424-1976 for further direction if during business hours or call Michael Garron Hospital Triage at 416 469 6580 extension 6216
- When paging, give your first and last name, the name of one of your midwives and/or their team colour, your phone number, the date your baby is due, and the reason why you are paging
Choice of Birthplace
HOME
Midwives are fully trained to attend births in the comfort of your own home for those who are low-risk. All midwives carry birth and emergency equipment – equivalent to a Level 1 hospital in Ontario. Midwives take care of home birth set up and clean up. Non-medical pain relief options available. Out-of-hospital birth info night offered at TMC, see “Prenatal Classes”.
TORONTO BIRTH CENTRE
(416) 366-8080
www.torontobirthcentre.ca
Fully regulated healthcare facility run by midwives, which provides birthing services free of charge. Clients wishing to register at the TBC will fill out a registration form with their midwife during a prenatal appointment.
To book a tour, call 416-366-8080 ex 101 or select option 3.
Non-medical pain relief options and nitrous oxide available.
Out-of-hospital birth info night offered at TMC, see “Prenatal Classes”.
MICHAEL GARRON HOSPITAL
825 Coxwell Ave(416) 461-8272
www.tegh.on.ca
Previously Toronto East General Hospital
All TMC clients must pre- register at MGH regardless of planned birthplace. You will be given a registration package at one of your prenatal appointments. If you do not have OHIP, your midwife will explain how to organize a payment plan with the hospital.
Non-pharmacological pain relief options and epidural available.
Obstetricians, anaesthetists & paediatricians on site.
Prenatal Classes
| Location | Contact | Cost | Notes |
|---|---|---|---|
| Midwives Clinic of East York- THE PRENATAL run by Sarah Lesie | sarahleslierm@gmail.com for more info and classes see: https://www.sarahleslie.ca/ |
$100/couple or $50/person | Led by our very own- Sarah Lesie! |
| Bloom Prenatal and Postpartum Support | Kama Lee Jackson 416-460-9909 Bloomtoronto.ca |
See website | Led by trained midwife |
| YOGA MAMAS (Queen & Greenwood) | 416-406-0116 www.torontoyogamamas.com |
$375 + HST/couple | Prenatal Birth Education and Movement Program, 6 week course |
| Access Alliance (Danforth & Vic Park) | 647-258-9782 | Free | Thursdays from 11:45 am - 1:00 pm |
| Better Beginnings (Finch & Don Mills) | Christina Yu 416-499-3377 |
Free | Many languages, book by 28th week, food & TTC tokens provided |
| Childbirth Joy – Prenatal Hypnosis (West Toronto) | Shawn Gallagher 416-255-8333 Childbirthjoy.com |
$330/couple | English, West Toronto |
| East York Family Resources (various locations) | 416-686-3390 Ext 9782 Worthyourweight.ca |
Free | Prenatal and ESL prenatal on Thursday |
| Hypnobirthing or Journey Into Childbirth | Jennifer Elliott 416-462-1938 Lifesjourney.ca |
$300 (hypno) & $195 (journey) +HST/couple | English |
| Midwifery Care North Don River Valley (Bathurst & Finch) | Sam Leeson Samleeson@gmail.com |
||
| Queer Positive Prenatal Class (519 Church St) | Chris Veldhoven 416-355-6780 519.org |
$125/person + $25 for manual | |
| Riverdale Community Midwives (Queen & River) | Jessica 416-922-4004 |
$150/couple | English |
| Michael Garron Hospital (Coxwell & Mortimer) | https://www.tehn.ca/programs-services/family-birthing-centre/prenatal-classes |
FREE | |
| Toronto Public Health (Many locations & ONLINE) | 416-338-7600 Toronto.ca/health/pregnancy |
Free | Register early |
| Prenatal Classes for Couples | Justine Sipprell 647-962-1563 Justine.sipprell@gmail.com |
$80/couple | Once a month on a Saturday from 2-5pm |
ADDITIONAL CLASSES (Ask your midwife for more information)
- See our latest classes at the Midwives’ Clinic
- Out-of-hospital birth info night @ The Midwives’ Clinic
- Vaginal Birth After Cesarean (VBAC) info class @ Michael Garron Hospital
Fetal Growth & Development
| Week | Description |
|---|---|
4 Weeks |
|
8 Weeks |
|
12 Weeks |
|
16 Weeks |
|
20 Weeks |
|
24 Weeks |
|
28 Weeks |
|
32 Weeks |
|
36 Weeks |
|
40 Weeks |
|
Common Discomforts of Pregnancy
| Discomfort | Cause(s) | Suggestions |
|---|---|---|
| Backache |
|
Practice good posture. Avoid sitting/standing for long periods. Exercise frequently and wear proper footwear. Consider prenatal exercise or yoga class. Consider seeing a massage therapist, chiropractor, physiotherapist, osteopath or acupuncturist. Tylenol (Acetaminophen) can alleviate back pain and is safe to take in pregnancy. Page your midwife if you are preterm and having back pain that is coming and going in a pattern, especially if accompanied by cramping or vaginal bleeding. Page your midwife if you are experiencing back pain associated with urinary tract infection symptoms and/or fever. |
Breast Changes:
|
|
Wear a supportive bra and avoid bras with an underwire. Avoid soap on nipples as it can dry out skin. If you are leaking colostrum (first milk), allow nipples to air dry. If you discover a lump in your breast, inform you midwife at your next appointment and see your family doctor. |
| Constipation |
|
Exercise and hydration (6-8 glasses of water/day). Add fiber to your diet (i.e. fruits/veggies, whole wheat, ground flax, beans) or consider taking Metamucil. Consider adding healthy fats (i.e. extra virgin olive oil, flax oil) to meals. Dried prunes, prune juice, plain yogurt and probiotics may also be helpful. A stool softener such as Senokot or Colace is safe in pregnancy but should not be used for longer than 7 days. |
| Common Cold |
|
Rest & hydration. Use humidifier. Drink hot water with lemon & honey. Gargle salt water or try lozenges. Echinacea root tincture: 1 drop/4lbs of your body weight every 4h. Consider Benilyn DM, a safe cough medication in pregnancy. Consider nasal saline spray (Salinex) for a few days. If you experience seasonal allergies, Benadryl (Diphenhydramine) is safe in pregnancy. |
| Dizziness |
|
Stay hydrated and do not skip meals. Stand up slowly. Rest frequently. Increase iron in diet (see Anemia section). If you are experiencing frequent dizziness, inform your midwife. Page your midwife if you are experiencing vision changes and/or severe headache. |
| Frequent Urination |
|
Kegel exercises – squeeze muscles around vagina as if you were trying to stop the flow of urine, then relax. Stay hydrated and empty bladder frequently. Call the clinic and leave a message for your midwife if frequent urination is accompanied by: painful urination (burning), blood in urine, urgency, pelvic pressure. |
| Groin Pain |
|
When getting up from lying down, draw knees up then role to side. Bend forward when laughing or sneezing. Rest & consider heating pad or ice pack, Tylenol (Acetaminophen) or support belt. |
| Headache |
|
Rest & hydration. Cold cloth on forehead. Try Tylenol (Acetaminophen). Try warm bath and/or neck & shoulder massage. Page your midwife if you have a severe/long-lasting headache or if accompanied by vision changes and/or pain in upper abdomen. |
| Heartburn |
|
Stay hydrated & try small frequent meals. Add raw almonds or plain yogurt after meals. Avoid fats. Sit upright after eating. Use pillows to sleep in upright position. Try Tums, Rolaids or Gaviscon if mild. |
| Hemorrhoids (Varicose veins in the rectal area) |
|
Treat constipation. Drink lots of water. Consider ice pack with witch hazel. Try preparation H or Anusol. Inform your midwife if you have hemorrhoids, especially if they are severe or causing increased discomfort. |
| Itching |
|
Exercise & hydration. Warm bath with oatmeal. Moisturize with lotion. Apply vitamin E or coconut oil to affected area. Try introducing fish oil supplement. Inform your midwife if you have a rash, and consider a visit to your family doctor. Inform your midwife if you are having severe itching, especially on palms or soles of feet. |
| Leg Cramps |
|
Increase calcium (dairy products, leafy greens, beans, almonds), magnesium (fruits, nuts, beans, soy) and potassium (banana, avocado, spinach) in diet or consider supplement. Exercise & hydration. Take a warm bath and consider Tylenol for pain. When you have a leg cramp, straighten your leg & flex your toes, massage the cramp and try and walk it off. Try a heating pad. Page your midwife if you have a hot, red, painful spot on your leg as this may indicate a blood clot. |
| Mood Changes |
|
Talk about your feelings. Continue doing activities that make you happy. Take time for yourself. Exercise & nap regularly whenever possible. Maintain a healthy diet. Consider a pregnancy support group. If you are concerned that you may be experiencing depression or anxiety, please inform your midwife at the next appointment. Page your midwife if you are having thoughts of harming yourself. See Additional Resources for more info. |
| Nausea & Vomiting |
|
Small frequent meals to keep stomach full. Stay hydrated. Eat crackers or yogurt before getting out of bed in the morning. Increase protein in diet (meat, vegetables, beans). Consider “Sea Bands”. Ginger, dandelion root/peppermint teas may also be helpful. Try vitamin B6 or Gravol, which is safe in pregnancy. If you are experiencing severe nausea & vomiting inform your midwife and ask about Diclectin. Page your midwife if you are experiencing nausea and vomiting accompanied by a severe headache, severe pain, dizziness and/or fever. |
| Nosebleeds |
|
Increase vitamin C in diet. Try a humidifier. Consider Nozohaem gel or small amount of petroleum jelly / vitamin E ointment in nostrils. |
| Numbness/Tingling |
|
Hydration, light stretching and movement of affected area. For carpal tunnel syndrome, consider wrist splints and rotation/stretching of the hands and wrists. Try using pillows to aid in positioning (i.e. under belly & between legs) when sleeping. |
| Swelling |
|
Drink 6-8 glasses of water/day. Elevate legs as much as possible. Consider support stockings. Exercise regularly (swimming is great for circulation). Avoid sitting with legs crossed. Try Epsom salt bath. Nettle/dandelion leaf infusion (1-2c/day). Inform your midwife if you are experiencing severe swelling. Page your midwife if you are experiencing swelling (especially in face) accompanied by headaches or vision changes. Page your midwife if you notice a hot, red, painful spot on your leg as this could indicate a blood clot. |
| Tiredness |
|
Rest as much as possible. Plan for extra supports during the end of pregnancy. Exercise daily. Eat small, well-balanced meals. If you suffer from insomnia, consider a warm bath before bed and/or meditation/relaxation techniques. Inform your midwife if you have dizziness/headache. |
| Vaginal Discharge (Increased vaginal discharge is common, especially at the end of pregnancy. Usually clear/white) |
|
Wear cotton underwear. Avoid vaginal douching. Consider eating yogurt daily or taking a daily probiotic to promote healthy vaginal bacteria. Call the clinic and leave a message with your midwife if you are experiencing vaginal burning or itching, abnormally coloured (green/grey) or foul-smelling discharge. Vaginal suppositories (Canesten & Monistat) for yeast infections are safe in pregnancy and may be recommended by your midwife. Natural remedies for yeast infections include: 1tbsp apple cider vinegar/day in glass of water, reducing sugar intake and plain live culture yogurt on vagina to relieve itching. If you think your water has broken (large amount of fluid continuously leaking from vagina, usually soaking a pad), page your midwife. |
This information is partially derived from www.monroeclinic.org and www.babies.sutterhealth.org
Herbal Recipes for Pregnancy
By: Aviva Romm
Rich in iron, calcium, trace minerals, ++vitamins and helpful in the postpartum too.
- 2 parts red raspberry leaf
- 2 parts nettle
- 1 part oatstraw
- ½ part alfalfa
- ½ part rosehips
- ¼ part red clover
- ¼ part spearmint leaf
- Pour 1L of water over ¼ cup (handful) of herbs and steep, covered for 30 minutes to 2 hrs.
- Drink 1 – 4 cups per day.
By: Aviva Romm
- 1 part Chamomile flowers
- 1 part Lemon balm
- ½ part Lavender flowers
- Use 1 tbs for a big cup of tea, steep 10-15 min.
- 2. Drink up to 2 cups per day.
By: Kat Montgomery, RM
- 3 parts Nettle
- 3 parts Raspberry leaf
- 2 parts Alfalfa leaf
- 1 part Mint
- ⅓ cup maple syrup
- ¼ tsp sea salt
- 2 Ca/Mg tablets, crushed
- ⅓ cup fresh lemon juice
- Make a strong infusion from the herbs by pouring 1 L boiling water over a large handful of herbs and steep 30 min to 2 hrs, covered.
- Strain and while warm (gently re-heat if needed) add maple syrup, crushed tablets and sea salt. Stir until dissolved.
- Cool to room temp, add lemon juice.
- Put in freezer for 2 hours then remove and stir to make a mush.
- Refreeze until you are ready.
Exercise & Nutrition
Adequate nutrition and exercise are important in maintaining a healthy pregnancy. The following information is partially derived from The Government of Canada.
Take a prenatal vitamin once daily. This vitamin should include folic acid (0.4mg unless specified by your care provider). Folic acid is essential for normal development of the baby’s spine, skull and brain, especially in the first month of pregnancy.
Ensure adequate iron intake. Make sure your prenatal vitamin contains between 16-20mg of iron. Consider increasing iron in diet (see Anemia section).
Follow Canada’s Food Guide to eat the right amount and type of food for you and your baby. Pregnant people need 2-3 additional food servings from any of the main food groups each day.
Avoid foods/drinks that are high risk during pregnancy (see below for some examples).
Maintain regular exercise habits in pregnancy. Pregnancy is not the time to try a high-impact or intense exercise for the first time. If you are used to intense exercise, listen to your body and modify as needed. Talk to your midwife if you have concerns about your exercise habits. If you do not exercise outside of pregnancy, start slow. We suggest low-impact exercises such as: prenatal yoga, swimming and/or walking. Exercise can help improve mood, ensure appropriate weight gain, promote sleep, increase strength and help to build your stamina for labour and delivery.
Stay hydrated throughout the day and especially while exercising.

WHAT TO AVOID IN PREGNANCY
Food & Drink
- Raw fish and shellfish
- Undercooked meat or seafood
- Hot dogs, non-dried deli meats, meat spreads and refrigerated smoked fish
- All foods made with raw and/or lightly cooked eggs
- Unpasteurized and pasteurized soft cheeses such as Brie or Camembert and unpasteurized semi-soft cheeses such as Roquefor or Stilton
- Unpasteurized juices, such as unpasteurized apple cider
- Raw sprouts (i.e. alfalfa sprouts)
- Alcohol – there is no known safe amount in pregnancy
- Caffeine – 1-2 cups a day is likely safe in pregnancy
Herbs
- Aloe Vera (topical okay in moderation)
- Black cohosh
- Blessed thistle
- Blue cohosh
- Buckthorn bark
- Calendula (small amount topical, okay)
- Coltsfoot
- Comfrey (small amounts topical okay after first trimester)
- Dong quai
- Duck root
- Ephedra (ma huang)
- Evening Primrose (oil is okay)
- Feverfew
- Ginseng
- Goldenseal
- Gotu kola
- Juniper berries
- Labrador tea
- Licorice
- Lobelia
- Nutmeg (okay in food)
- Parlsey (okay in food)
- Pennyroyal
- Rosemary (okay in food or used in bath as essential oil)
- Sage (okay in food)
- Sarsparilla
- Sassafras
- Senna
- Shepards’ purse
- Uva Ursi
- Yarrow
Other
- Street drugs
- Prescription pain meds
- Opioids
- Cannabis
WEIGHT GAIN IN PREGNANCY
Recommended weight gain in pregnancy is based on Body Mass Index. This is not a perfect measurement as it does not consider bone structure, muscle mass and genetics. There are many BMI calculators online or you can use the formula: Weight (in kilograms) ÷ Height (in meters)² = BMI
Recommended weight gain according to Society of Obstetricians and Gynecologists of Canada (SOGC):
- BMI Before PregnancyRecommended Weight Gain
- Less than 18.512.5 to 18 kg (28 to 40 lb)
- Between 18.5 and 24.911.5 to 16 kg (25 to 35 lb)
- Between 25 and 24.97 to 11.5 kg (15 to 25 lb)
- More than 30At least 7 kg (15 lb)
- Twin pregnancies16 to 20.5 kg (35 to 45 lb)
Obesity in Pregnancy: What Are the Risks?
Having excess weight before pregnancy, particularly a BMI over 30, can increase your risk of serious health problems and is linked with many complications in pregnancy that affect you and your baby.
Risks for You
- Gestational diabetes
- Gestational hypertension
- Caesarean section (& increased risks for complications)
- Increased risk of excessive blood loss
- Early labour & birth
- Miscarriage
- Infertility
- Baby growing too big (difficult delivery)
- Difficulty monitoring fetal heart rate
- Needing to stay in hospital after birth
- Birth defects, including neural tube defects
- Stillbirth
This information is directly from the SOGC’s Pregnancyinfo.ca
CANADA’S FOOD GUIDE

EXERCISE & NUTRITION RESOURCES
Government of Canada - Canada.ca
- Healthy Weight Gain During Pregnancy
- Prenatal Nutrition
- Pregnancy And Breastfeeding
- Physical Activity & Pregnancy
- Eating Well with Canada’s Food Guide
The Sensible Guide to a Healthy Pregnancy Healthycanadians.gc.ca
Society of Obstetricians and Gynaecologists (SOGC) (See: Healthy Eating, Exercise and Weight Gain Before and During Pregnancy)
Dietitians of Canada Dietitians.ca
City of Toronto Healthiest Babies Possible (free one-to-one nutrition counseling)
Vaccinations in Pregnancy
The recommendation is that everyone who is considering pregnancy be fully up to date on their routine vaccinations. Many vaccines are not recommended during pregnancy because of the risk to the baby. In Ontario, there are two standard recommended vaccines in pregnancy. Your care provider may recommend other vaccines depending on your individual circumstances.
1. INFLUENZA VACCINE (“Flu Shot”)
Pregnant people are at higher risk of flu complications due to changes in the immune system. The flu shot is publicly funded in Ontario – get yours at: a pharmacy, family doctor, walk-in clinic or public health clinic.
Check out: Ontario.ca
2. TDAP VACCINE (“Pertussis” or “Whooping Cough”)
Includes protection against tetanus, diphtheria and pertussis.
The recommendation is to receive Tdap in every pregnancy regardless of previous vaccinations. This is to protect your baby against pertussis from birth until they receive their own vaccination.
Tdap is recommended between 21-32 weeks of pregnancy and can be given by a family doctor or nurse practitioner.
For more information, visit Canada.ca
Prenatal Assessments
INITIAL BLOOD WORK
- CBC (iron & platelet levels)
- Group & Screen (blood type + antibodies)
- Random Glucose
- Public Health Blood Work
- Hepatitis
- Rubella
- Syphilis
- HIV
- Additional tests if clinically indicated
- Ferritin (iron stores)
- Thyroid stimulating hormone (TSH)
- Immune status of infectious diseases (i.e. parvo B19, CMV, toxoplasmosis, chicken pox)
URINE TESTS
- Urine sample to test for urinary tract infection (UTI)
- Urine sample to test for Gonorrhea & Chlamydia infections
- Urine dip stick for protein & glucose, if clinical indicated
ADDITIONAL INVESTIGATIONS (As Needed)
- Vaginal Swabs for infections:
- Yeast
- Bacterial Vaginosis
- Sexually Transmitted Infections (STIs)
- Additional CBC for hemoglobin (iron) monitoring (It is recommended that all pregnant clients receive a repeat CBC around 30-32 weeks to ensure iron level is appropriate in time for delivery.)
DATING ULTRASOUND
- Performed during the first trimester
- Fetus is measured from head to rump (crown-rump length) to determine the most accurate estimated due date.
- This ultrasound also confirms the number of fetuses.
SECOND TRIMESTER ULTRASOUND (Anatomy Scan)
- Performed between 18-20 weeks, preferably after 19 weeks
- Ultrasound tech and radiologist will analyze baby’s full anatomy – bones, organs, measurements, sex (optional) etc.
- The location of the placenta is determined to ensure it is not covering the opening of the uterus (the cervix).
CERVICAL CANCER SCREENING (Pap Test)
- Screening guidelines are set by The Ontario Cervical Screening Program.
- It is recommended that those who have been sexually active have a Pap test every 3 years beginning at age 21.
- More frequent Pap tests may be recommended if the results are abnormal.
- An instrument called a speculum is gently inserted into the vagina to be able to see the cervix. A sample of cells is taken from the cervix and tested for signs of cervical cancer.
- A pap test can be performed in pregnancy up to 20 weeks if a client is due for their routine screen. Registered Midwives are trained to do Pap tests and will offer in pregnancy or at 6 weeks postpartum if warranted.
For more information about cervical cancer screening, or Ontario’s Cervical Screening Program call 1-866-662-9233, visit Ontario.ca or Cancercareontario.ca
GESTATIONAL DIABETES SCREENING
Gestational Diabetes is diabetes that develops in pregnancy and affects how your body manages sugar.A screening for gestation diabetes is recommended in every pregnancy. This screen will identify those at higher risk of developing gestational diabetes. The screening is called the Oral Glucose Challenge Test (OGCT) and can be completed at TMC with your midwife between 24-28 weeks of pregnancy.
For the OGCT, your midwife will ask you to come 45 minutes to 1 hour before your scheduled appointment, at which point you will be given a glucose drink. One hour after you are finished the drink, your midwife will take a blood sample to see how your body manages the sugar. We ask that you refrain from eating for 1 hour before the test and avoid foods with high sugar that day.
If the screening comes back positive, you may be at risk of having gestational diabetes. Your midwife will offer a follow-up diagnostic test, called an OGTT. Usually, gestational diabetes can be managed through diet and exercise to control blood sugar. Occasionally, gestational diabetes requires the client to take insulin. If it is diet-controlled, the client is still suitable for midwifery care, though your midwife will recommend a consultation with an obstetrician and the gestational diabetes clinic at MGH. If insulin is needed, the care will be transferred to an obstetrician for the remainder of the pregnancy.
Those at higher risk of gestational diabetes include: clients older than 35, gestational diabetes in a previous pregnancy, family history of diabetes or gestational diabetes, high BMI (30+), previous baby over 9 pounds or with birth defect, non-white race, polycystic ovarian syndrome and a previously unexplained stillbirth or miscarriage. Some clients who are not at high risk may choose to decline this screening after discussing risks/benefits with their midwife.
For more info, please visit Diabetes.ca
GENETIC SCREENING
Prenatal genetic screening is an OPTIONAL screening that is offered to all pregnant clients in Ontario. Your midwife will discuss with you the options for genetic screening at your first appointment. Please keep in mind; the following screening options are NOT DIAGNOSTIC of the conditions listed below. These tests are simply used to determine which pregnancies are at higher risk of being affected. If a prenatal screen comes back positive, meaning the pregnancy may be affected; your midwife will offer a consult with a genetic counselor to discuss options for further testing if you wish.
| Screening Option | Conditions Screened | When | How | Accuracy | Additional Information |
|---|---|---|---|---|---|
| First Trimester Screen (FTS) | Down Syndrome (Trisomy 21) Patau Syndrome (Trisomy 18) |
11+3 – 13+3 weeks | Ultrasound & blood test done on same day | T21 = 83% T18 = 91% |
|
| Non-Invasive Prenatal Test (NIPT) | Down Syndrome (T21) Patau Syndrome (T18) Edwards Syndrome (T13) |
Anytime after 10 weeks | Blood test | T21 = 99% T18 = 98% T13 = 80% |
|
| Maternal Serum Screen (MSS) | Down Syndrome (T21) Patau Syndrome (T18) Open Spina Bifida (OSB) |
15-20 weeks | Blood test | T21 = 81% T18 = 60-70% OSB = 85% |
|
| Anatomy Scan | Soft markers of physical abnormalities that may be indicative of genetic condition such as T21
Open Spina Bifida (OSB) |
18-20 weeks | Ultrasound | T21 = 40% OSB = 90% |
|
CONDITIONS
Trisomy 21 (Down Syndrome)
DNA has 3 copies of chromosome 21. People with Down Syndrome can live into their 50s & 60s. They often have congenital anomalies and intellectual disability.
Trisomy 18 (Patau Syndrome)
DNA has 3 copies of chromosome 18. Many affected fetuses will not survive to term. Of those who are born, average age of survival is 14 days.
Trisomy 13 (Edwards Syndrome)
DNA has 3 copies of chromosome 13. Most affected fetuses will not survive to term. Of those who are born, 90% will not survive their first year.
Open Neural Tube Defect (Open Spina Bifida)
Membranes that surround the brain/spinal cord fail to close. If this occurs at the top of the neural tube, the fetus often does not survive to term or past the first couple of days. If it occurs at the bottom, the baby will have spina bifida.
For more information, please visit: Prenatalscreeningontario.ca or Mountsinai.on.ca
Fetal Movement
People who are pregnant typically start to feel the baby’s movements between weeks 16-25. Many people describe early movements as a “flutter” or similar to gas.
Fetal movement becomes a reliable measure of fetal wellbeing after 28 weeks of pregnancy. At this point, you should feel a minimum of 6 fetal movements every 2 hours.
Babies do sleep and have periods of rest while in utero.
Daily fetal movement counting is NOT recommended for low risk pregnancies. If you are more than 28 weeks pregnant and are concerned about your baby’s movement, do a kick count.
What is a kick count and how do I do it?
- Reliable AFTER 28 weeks of pregnancy & should only be done if you are concerned that your baby’s movements are absent or have decreased.
- Stop what you are doing and find a quiet place to sit/lie down.
- Have a cold drink of water or something sweet and place your hands on your belly.
- Focus on counting the baby’s movements (kick, roll etc.).
- Stop counting once you have felt 6 movements. If two hours pass and you have not felt 6 movements, page your midwife.
Preterm Labour Symptoms
Preterm labour is labour occurring before 37 weeks of pregnancy. Factors such as smoking/drug use, previous preterm birth, infection and trauma can increase the risk of preterm labour. In 50% of preterm labour cases, the cause is unknown. If you are experiencing symptoms of preterm labour, page your midwife. A consultation and/or transfer of care to an obstetrician may be recommended.
SYMPTOMS OF PRETERM LABOUR
- Menstrual-like cramping in lower abdomen with increasing intensity, coming and going in a pattern. These cramps (contractions) do not go away with position changes, a bath or Tylenol.
- Blood or fluid leaking from the vagina.
- Back pain that is coming and going in a pattern.
- These symptoms may be accompanied by diarrhea, pressure in lower abdomen and/or nausea/vomiting.
TO REDUCE THE RISK OF PRETERM LABOUR
- Do not smoke in pregnancy or try your best to cut down as much as possible.
- Seek out prenatal care and discuss risk factors/concerns with your care provider.
- Take a prenatal class.
- Stay hydrated, eat a balanced diet and maintain an active lifestyle.
- Minimize stress-inducing and/or intense activities.
Anemia (Low Iron) in Pregnancy
The following information is directly from the Association of Ontario Midwives
WHAT IS IRON DEFICIENCY ANEMIA?
Iron plays many important roles in your health. You need iron to make hemoglobin, a part of red blood cells that carries oxygen throughout the body. When you have iron deficiency anemia, you don’t have enough iron to make hemoglobin, so your body starts to make smaller and fewer red blood cells. Less hemoglobin and fewer red blood cells also means your cells can’t get the oxygen they need.
NORMAL CHANGES TO BLOOD VOLUME IN PREGNANCY
Pregnancy causes many changes in the body. One of the changes that happens in pregnancy is that the amount of blood in your body almost doubles. Blood is made up of red blood cells, white blood cells and fluid called plasma. The number of red blood cells doesn’t increase as much as the plasma. This process is called “hemodilution” because the blood cells get diluted when the plasma increases. Hemodilution is a healthy response to pregnancy and a common cause of anemia. If your iron is low at the start of your pregnancy, this normal process of hemodilution can lead to anemia.
HEMOGLOBIN is a part of red blood cells. Hemoglobin carries oxygen throughout the body.
IRON is something your body needs in order to make hemoglobin. Iron is an essential nutrient, which means you have to get iron from your diet because your body can’t make it.
HEME IRON (also called organic iron) is found in meat. The body easily absorbs this type of iron.
NON-HEME IRON (also called inorganic iron) is mainly found in leafy greens, but is also found in meat, poultry and fish. This type of iron is less easily absorbed by the body.
FERRITIN is a protein that stores iron in your body. Your body can use the “backup” iron that is stored in ferritin when it doesn’t get enough iron from the food you eat.
HOW DO I KNOW IF I’M ANEMIC?
Having a blood test is the only way to know for sure if you have anemia. Your midwife will offer you a blood test to check your hemoglobin levels in early pregnancy and again around 30-32 weeks of pregnancy. You may be offered another blood test after your baby is born. Your midwife may also offer testing more frequently in pregnancy if there are concerns you might be anemic.
WHAT MIGHT INCREASE MY RISK OF HAVING ANEMIA?
A vegetarian or vegan diet may put you at higher risk for anemia because the iron found in vegetarian food sources is non-heme iron and is harder for the body to absorb.
Vitamin D deficiency may also increase the risk of anemia since vitamin D plays an important role in iron absorption. Your body produces vitamin D when your bare skin is exposed to sunlight. Anyone who keeps their skin mostly covered may be at higher risk of vitamin D deficiency. Because of our long winters, this can include most people who live in Canada!
A multiple pregnancy (twins or triplets) may put you at higher risk for anemia because the demands for iron are even higher than during a pregnancy with one baby.
It can take up to 18 months for the body to fully recover from a pregnancy, so two (or more) pregnancies less than a year apart can make it hard to maintain good iron stores.
People who have very heavy menstrual periods often have low iron because they lose a lot of blood every month. If you had heavy periods before becoming pregnant, you may be at higher risk of anemia during pregnancy.
If you are anemic during pregnancy you are also more likely to be anemic postpartum.
If you have a postpartum hemorrhage (losing too much blood after birth), you may be at higher risk for becoming anemic. For more information about postpartum hemorrhage, see Client Handouts page on OntarioMidwives.ca.
WHY TREAT ANEMIA?
It’s important to treat anemia so you feel better as quickly as possible and to maintain your overall health. It is also important to ensure that your iron levels are healthy if you are planning a future pregnancy. If your iron levels are very low in early pregnancy, there is a slightly higher chance that your baby will be born early or could be born smaller than expected (also called, “small for gestational age”). It is also important to treat anemia before you give birth. It is normal to lose some blood during labour and delivery, but low hemoglobin at the start of labour can put you at risk of worsened anemia after the baby is born. Depending on how severe your anemia is at the end of your pregnancy, your midwife may have recommendations about where you plan to give birth.
HOW IS ANEMIA TREATED?
If you are diagnosed with anemia, your midwife will discuss options for treatment. Iron pills or liquid supplements are usually the first choice to treat anemia during and after pregnancy.
There are lots of different iron supplements available in Canada. Iron is often included in multivitamins, including prenatal vitamins. Elemental iron is the form of iron that your body absorbs easily and different formulations of iron supplements contain different amounts of elemental iron. It is recommended that people who are diagnosed with iron deficiency anemia take supplements that provide about 50-100 mg of elemental iron each day.
There isn’t strong evidence showing that one brand of iron is more effective or causes less side-effects than any other. It can be confusing to choose which iron supplement to buy, especially since prices vary. Talk to your midwife about what supplement is right for you.
ACCESS TO IRON SUPPLEMENTS
Some health-care plans and Ontario Works will pay for over-the-counter medications (like iron) if a health-care provider writes a prescription. Check with your health plan or your Ontario Works caseworker to see if your iron supplements will be free or cost less with a prescription from your midwife.
DOS AND DON’TS FOR TAKING IRON
Iron is best absorbed on an empty stomach. Sometimes iron supplements can give you a stomach ache, make you constipated or give you diarrhea. If you are having unpleasant side-effects from taking iron, you can try taking iron right after meals instead of on an empty stomach, or try taking it before you go to bed. You can also talk to your midwife about starting at a lower dose and gradually increasing the dose. It is normal to notice dark coloured bowel movements when you are taking oral iron.
- DO take your iron with vitamin C (citrus fruits like oranges, strawberries, tomatoes, or a 500-mg vitamin C tablet). Your body needs vitamin C in order to absorb iron.
- DO keep taking iron supplements for at least three months even if you start to feel better, unless your midwife gives you different instructions. Your symptoms might improve quickly, but taking iron for the full three months ensures that you replenish your iron stores (ferritin).
- DO talk to your midwife if the side-effects of iron are bothering you.
- DO make sure that iron supplements are kept out of the reach of children. Iron can be toxic.
- DON’T drink coffee or black teas at the same time you take iron. Tannins in coffee and tea stop your body from absorbing iron. Wait at least one hour after taking iron to have tea or coffee.
- DON’T take your iron along with calcium. Avoid eating dairy (milk, yogurt, cheese), or taking calcium pills, or antacids (like Tums) within about an hour of taking iron supplements. Try to avoid combining iron-rich foods with foods rich in calcium (like dairy products). Calcium gets in the way of your body’s ability to absorb iron.
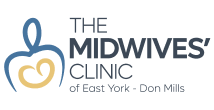
BOOSTING THE IRON IN YOUR DIET
If your midwife has diagnosed you with anemia, then food sources alone probably won’t be enough to improve your anemia. But it still helps to try to eat iron-rich foods as much as you can along with any supplements you may be taking. Dieticians of Canada has good information about iron and iron-rich foods. Please see: Dietitians.ca.
ACCESS TO HEALTHY FOODS
If you are pregnant or have just had a baby and are receiving Ontario Works, you are eligible for an extra $40 a month through the Pregnancy/Breastfeeding Nutritional Allowance. Midwives can complete forms provided by Ontario Works caseworkers to access this funding for you.
OTHER TREATMENT
If your anemia is severe, or if it’s not getting better after you have tried oral iron supplements, your midwife may discuss a consult with an obstetrician to discuss other treatment options like getting iron through an IV (a needle in your arm).
ANEMIA AND DEPRESSION
The symptoms of anemia can sometimes be similar to symptoms of depression. If you are anemic either during your pregnancy or after your baby is born, you may feel like you are depressed. Anemia can also lead to depression. If you have any concerns about the symptoms below, talk to your midwife.
| IRON DEFICIENCY ANEMIA Symptoms | DEPRESSION Symptoms |
|---|---|
|
|
IRON RICH FOODS
| Food | Serving Size | Iron (mg) |
|---|---|---|
Fruits & Vegetables
|
|
|
Grain Products
|
|
|
Meat Products
|
|
|
Fish & Seafood
|
|
|
Meat Alternatives
|
|
|
Other
|
|
|
NOTES & RESOURCES
Pregnant people should limit intake of liver to one serving every two weeks.
Iron is best absorbed when consumed with foods that contain vitamin C.
Calcium should be avoided when eating iron rich foods as it inhibits the body’s absorption of iron.
Caffeine may also inhibit iron absorption.
Association of Ontario Midwives – Iron Deficiency Anemia
Group B Strep (GBS)
The following information is derived from the Association of Ontario Midwives – Clinical Practice Guidelines
WHAT IS GBS?
GBS is a type of bacteria that is a normal part of body flora. At any given time, about 10-35% of people who are pregnant have GBS in their vagina and/or rectum. GBS is not usually harmful to an adult and most people who have the bacteria will not have any symptoms.
WHY ARE WE CONCERNED WITH GBS?
GBS can cause sickness in babies in their first week of life (early-onset) or after the first week (late-onset).
The most common ways that babies get GBS is from the birthing parent during labour & birth.
Though most babies are unaffected, a small number of babies exposed will develop a GBS infection. This can lead to bacteria in the blood (sepsis), lung infection (pneumonia), inflammation in the brain/spine (meningitis), respiratory infections and death. Some babies will have long-term effects.
WHAT INCREASES MY BABY’S RISK OF GETTING EARLY ONSET GBS?
Your baby is at higher risk of early-onset GBS disease if one or more of the following occurs:
- You are GBS positive during labour or have GBS in your urine in pregnancy
- Your baby is born preterm
- Your baby weighs less than 2500 grams
- Your water breaks more than 18 hours before you baby is born
- You have a fever during labour
- You had a previous baby with GBS disease
HOW CAN I FIND OUT IF I CARRY GBS?
Your midwife will recommend a self-administered swab around 35-37 weeks of pregnancy to screen for GBS bacteria.
It is a vaginal-rectal swab that is considered valid for 5 weeks after testing. Your midwife will explain how to do the test.
If your test comes back positive, it means you carry the GBS bacteria at that time. If the test is negative, the bacteria is not present. This test correctly identifies someone with GBS 87% of the time.
As with all tests in pregnancy, GBS screening, though recommended, is not mandatory.
HOW CAN WE HELP PREVENT EARLY-ONSET GBS DISEASE?
If your baby is at risk (for example, if you are GBS positive), you will be offered IV (in the vein) antibiotics during active labour.
If you choose to take the antibiotics, a dose is given every 4-8 hours until your baby is born. Most antibiotics can be administered at home, hospital or birth centre.
With all antibiotics, there is a risk of disturbing beneficial bacteria in the body which can on occasion lead to a yeast infection. In rare cases, antibiotics may cause:
- Allergic reaction in pregnant person
- Antibiotic resistance (creating resistant bacteria)
- Possible increased risk of baby developing asthma or allergies.
- Swab for GBS and receives antibiotics if GBS positive.
- This option is currently the most popular in Ontario and in our community.
- With this, you will be offered antibiotics during labour if you test positive for GBS at 35-37 weeks.
- This choice reduces early-onset GBS disease in babies by 65-86% when compared to babies of clients who did not receive antibiotics.
- Swab for GBS and receives antibiotics only if GBS positive AND if there is another risk factor.
- With this option, you will be offered antibiotics in labour if you tested positive for GBS at 35-37 weeks AND:
- You go into preterm labour
- You develop a fever during labour
- Your water breaks before labour
- This choice reduces early-onset GBS disease in babies by 51-75% when compared to babies born to clients who do not receive antibiotics.
WHAT ARE MY CHOICES
The two most common ways of screening for and treating GBS are:
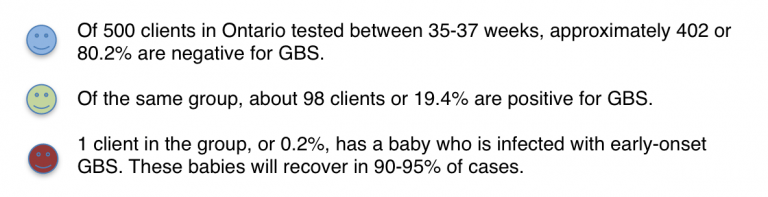
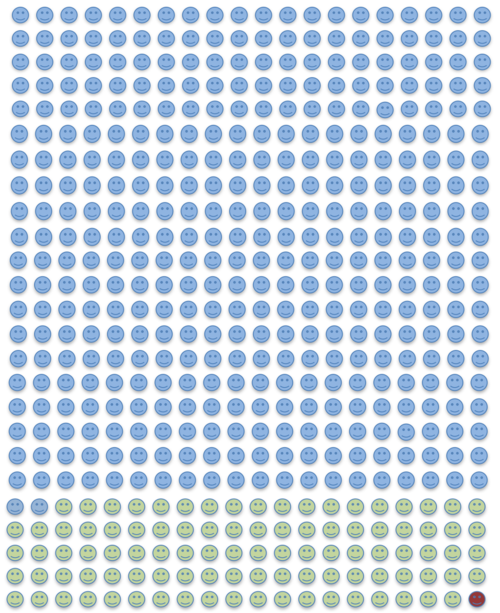
RISKS OF EARLY ONSET GBS DISEASE
The following graphic demonstrates a visual to help our clients understand the risks of their baby developing early onset GBS infection.
Additional Resources
HERBAL RESOURCES
Botanical Medicine for Women’s Health, Aviva Romm (2009)
The Natural Pregnancy Book, Aviva Romm (1997)
Naturally Healthy Babies and Children, Aviva Romm (2000)
Wise Woman Herbal for the Childbearing Year, Susun Weed (1985)
MENTAL HEALTH RESOURCES
MGH – Women’s Mental Health
Centre of Perinatal Excellence
RNAO Guidelines
PREGNANCY SYMPTOM RESOURCES
Monroeclinic.org
Babies.sutterhealth.org
EXERCISE & NUTRITION RESOURCES
Government of Canada
The Sensible Guide to a Healthy Pregnancy
Society of Obstetricians and Gynaecologists (SOGC)
Dietitians of Canada
City of Toronto Healthiest Babies Possible (free one-to-one nutrition counseling)
Iron Deficiency
CLINICAL RESOURCES
Vaccinations in pregnancy
GDM
Genetic screening: Prenatal Screening Ontario OR Mount Sinai
Cervical Screening: Ontario.ca OR Cancer Care Ontario
Indications for Consultations and Transfers of Care
CHOICE OF BIRTHPLACE RESOURCES
Research from British Colombia
The Association of Ontario Midwives “Choice of Birthplace”
The Association of Ontario Midwives “Birth Place Options”
BIRTHPLACE OPTIONS
You can download a PDF copy of our welcome package here.
Need a copy of our feeding log? Download a PDF copy here.
Frequently Asked Questions
-
No, you can’t have both a midwife and a doctor as your primary care provider. Midwives, obstetricians, and family physicians are all considered primary caregivers in Ontario. A primary caregiver is the person who is most responsible for your care. To have two primary caregivers is a duplication of health care services. However, if your pregnancy requires a consultation or transfer of care your midwife will consult the appropriate doctor or specialist, such as your family doctor, an obstetrician, pediatrician or lactation consultant. In most scenarios your midwife will still remain your primary care provider. Occasionally a transfer of care may be required and then your midwife will provide you with supportive care.
-
Sometimes your care will be transferred but your babies won’t or your baby’s care will be transferred and yours won’t. In these situations, the midwife will continue to be the primary caregiver for either you or your baby. In any transfer of care your midwife will remain in supportive care. She will answer any questions you might have and act as your advocate.
-
No. Midwifery care is fully funded through the Ministry of Health and Long Term Care.
-
You can fill out our intake form on our website as soon as you know you are pregnant. Our administrative staff will call you within a few days to book your initial appointment with your midwife. If you would feel more comfortable to do the intake over the phone, you are welcome to call, and one of our administrators will fill out the form with you. If you do the intake over the phone, you will still have to wait a few days to book your initial appointment, as we need this time to assign you to a midwife. Please call as soon as you are pregnant or know that you want a midwife, as we fill up very quickly and often have a waiting list. If you decide later in pregnancy to change from a doctor to a midwife, you can be accepted into care if there are spots available. We will request your records from your previous caregiver to continue your care.
-
Midwives are specialists in normal, healthy pregnancy, labour, birth and postpartum care. If you have a previous or current health problem please include it on your intake form. If you have a significant health problem a midwife will review your form and may call you to discuss this prior to an appointment being made.